Brain Tumours – General Considerations
General Anatomy and Function
Being told you may have a brain tumour is confronting. However, it needs to be stressed that there are many different types of tumours that can occur, some of which are curable and yet others that can be kept under control over the course of someone’s life. Even for those types for which there is currently no cure in many cases very significant inroads have been made in treatment leading to marked improvements in quality and quantity of life even within the scope of the last few decades of Dr Brennan’s practice.
The most important thing up front is to carefully assess the individual case including the clinical findings, arranging the appropriate tests, working out the treatment options, and giving the patient the time they need to understand the nature of the problem so that they can be a partner in the decision making for treatment to meet their own expectations.

Dr Brennan is highly trained and experienced in the surgical treatment of conditions of the brain including brain tumours

General Considerations
Symptoms:
Sometimes a brain tumour may be picked up incidentally on a scan done for some other reason before it produces any symptoms whatsoever. In other situation various symptoms may develop that point to a tumour being present.
The following symptoms are common although the list is not exhaustive and of course not all symptoms occur in every case.
i) Headache
Headache is a very common symptom of many different and diverse problems that range from stress, viral infections, migraine, sinus disease, blood vessel problems, and tumours. The vast number of patients with a headache will of course not have a brain tumour. However, headache with the following features may warrant further investigations:
- headache that is out of character to what someone would consider as a “normal” headache for them
- headache that is persistent over time, certainly if it is progressive or getting worse as time passes
- a pattern of headache that is varies over the course of the day particularly if it tends to be worse in the mornings or wakes someone up from sleep
- headache that is associated with other symptoms such as blurred vision, nausea, or vomiting
ii) Neurological symptoms
- loss of visual awareness with the tendency to bump into things which were not seen
- weakness or sensory disturbance down one side or part of one side of the body
- memory, personality, or other so called “cognitive” changes
- unsteadiness or balance dysfunction that may affect walking
- loss of sense of smell often experience as food tasting more bland
- new difficulty with discreet complex tasks such as mathematics, coordinated actions, etc.
iii) Epileptic seizures
Seizures can come in various patterns. Some are easily recognisable as abnormal including generalised convulsions. Others may be more limited and restricted to one part of the body, move from one part to another, involve twitching or sensory changes, or sometimes more complex and unusual actions such as seemingly coordinated but inappropriate movements, abnormal smells, and periods of blankness or lack of engagement.
Seizures are a symptom of the brain being irritated by something, not always a brain tumour. In children they are commonly due to so-called primary epilepsy. However, in an adult who has never had seizure before a first onset seizure needs to be further investigated with scans and other tests since it may well mean an underlying tumour or other structural abnormality is developing in the brain.
Treatment options vary considerable depending on the diagnosis and the results of the initial investigations.
Investigations:
Each case is different and may need different tests to best work out what is happening and what treatment is required. It is important to tailor the investigations to the particular case at hand. In general terms however the following tests may be needed.
i) CT scan
This can be a readily accessed an inexpensive test to detect a structural problem with the brain. A modern CT scan often done both on its own and after the injection of some iodine based X-ray dye can pick up many of the more common and obvious tumours that may occur. As such it has some value as a screening test.
However, it may miss more subtle abnormalities and has a lower fidelity and definition than MRI. Also, it works with x-rays so that even though more modern machines have low dose modalities this test will still expose a patient to a small amount of radiation. Hence, although it can add information and reveal bone anatomy more clearly is not a test we would want to do too often if possible.
ii) MRI scan
Magnetic resonance imaging or MRI is the test of choice to identify structural problems with the brain. It provides the best resolution and definition available and so reveals with greater precision the extent of any abnormality detected. It is also safe in that it does not involve the use of X-rays but instead works on high strength magnetic fields. When dye is required this is non-ionic and does not have any cross reactivity with other types of X-ray dye. As such, in addition to being safer up front it is also more useful for surveillance or check-up type imaging since it can be done repeatedly without the downside of exposing the patient to too much cumulative X-ray type radiation.
There are some nuances however, with there being no such thing as a “standard” MRI. Different pictures or “sequences” are taken depending on the type of problem being investigated so that an MRI being done to investigate a tumour may include different pictures from that looking into stroke, epilepsy, aneurysm, multiple sclerosis, etc. It may be necessary to have more than one scan to complete all of the sequences required in an individual case.
Certain sequences in an MRI may also give some clues as to what type of tumour has been detected. Specialised modalities including MRI perfusion scanning give an indication of blood flow and possibly tumour activity, and MRI spectroscopy can give information as to relative concentration of various chemical metabolites that are within a specific portion of the tumour which may allow prediction of what cell types are present and therefore what type of tumour is being dealt with.
Some drawbacks include that the tunnel is more narrow than that for a CT and so people who have claustrophobia may need mild sedation to have the scan done. It also takes more time to perform, is very motion sensitive, and make enough noise that patients will be given ear plugs or headphones during the test. Also, due to the high strength magnetic fields nothing iron based can be brought into the room, and some patients with older pacemakers, cardiac defibrillators, or other metal foreign bodies (either surgically implanted or as a result of trauma) may not be able to have an MRI.
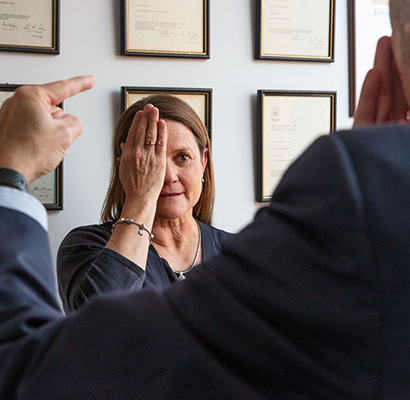
iii) FMRI
This is a dedicated type of MRI looking to map areas of function in the brain (the “f” stands for “functional”). This can be a useful tool to help plan surgery particularly for tumours which look to be closely associated with functioning or eloquent areas of the brain. The test is performed by a neuroradiologist inside an MRI machine with the patient being asked to perform simple tasks such as tap a finger, move a foot, or speak simple phrases while the scan is being performed. Expertise is required to know how and when fMRI will be useful.
iv) PET scan
Pet scan (which stands for Positron Emission Tomography) is a very specialised test that attempts to look at the activity of cells within a tumour. A radioactive isotope is used to label a chemical that the cells may be using as a metabolite such as glucose (in FDG PET imaging for example). As a general rule the more active a cell is the more it will use the metabolite and therefore show up as “hot” on the PET scan images.
There are many nuances and some exceptions to this general principle, however, and interpreting the results of the PET requires expertise and experience.
v) Multimodality Imaging
Multimodality imaging refers to combining some or all of the above tests on a workstation to interpret the results when combined. Each one test on its own will have various positives and negatives, but more information and power can be brought when the results are combined and interpreted together, often in the context of MDT meetings.
vi) Blood Tests
Blood tests will often be ordered in preparation for a general anaesthetic as part of a complete workup that may also include a chest x-ray and an electrocardiogram. Rarely, blood tests may be sent for so-called tumour markers, chemicals that a tumour may secrete into the blood and indicate what type of tumour is present. Currently, this is rare for adult tumours, but research projects are underway looking at various markers that in the future may help to make a diagnosis without the need for biopsy or surgery.
vii) EEG
Electroencephalogram or EEG is a test whereby a neurophysiologist can map brain waves via electrodes that are placed on the scalp. EEG has a place in cases where epileptic seizures are an issue, but generally speaking modern imaging modalities like MRI and PET have made EEG not as important in the investigation of possible brain tumour.



