General Considerations
General Anatomy and Function
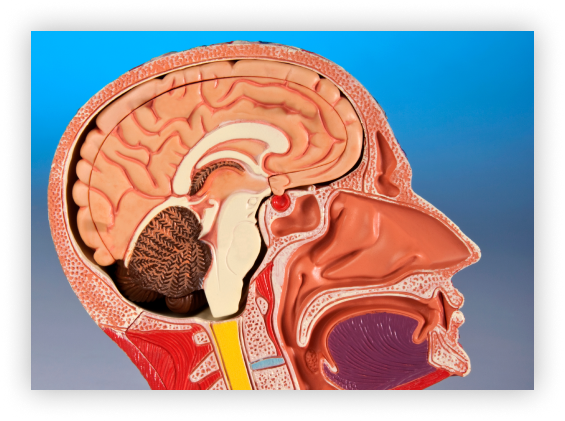
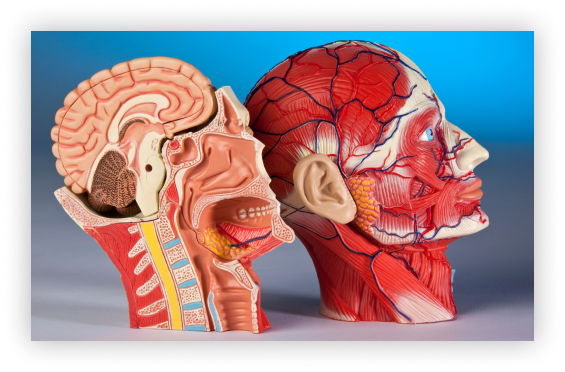
The pituitary gland is a small organ that sits underneath the base of the brain and immediately above the back of the nose (on top and behind of one of the nasal sinuses called the sphenoid sinus) in a pocket within the skull called the pituitary fossa or sella turcica (since it reminded early anatomists of a Turkish saddle).
Its location is explained by the fact that the front two thirds of the gland (the anterior lobe) develops in the embryo from the roof of the nose and the back one third (the posterior lobe) from the brain itself, with a small cleft known as Rathke’s cleft in between. The posterior lobe remains connected to the brain by the pituitary stalk.
The gland is surrounded by a rich collection of blood vessels and is bordered on each side by the cavernous sinuses through which run the carotid arteries on their way to supply the brain with blood and a variety of nerves that help move the eye and control sensation in the face. Immediately above the sella in the “suprasellar cistern” the optic nerves run back from the eye to the brain, meeting together in the middle and forming the optic chiasm. There is therefore a log jam of important structures in the immediate vicinity of the pituitary gland that may become involved in various disease processes.
The gland itself is sometimes referred to as the body’s master gland since it produces a number of hormones that help control other glands in the body such as the thyroid gland, the adrenal gland, and the gonads (ovaries in women and testes in men). It also has a function in regulating growth, the production of breast milk, and the salt concentration of the blood and body by influencing the ability of the kidney to concentrate urine.

Hormone production is a delicately balanced affair with the pituitary gland being part of a complex system of control and feedback to ensure that enough of any particular hormone is made at any particular time or condition. All of this means it is a very important part of the complex way our bodies maintain so called “homeostasis” (which broadly means keeping conditions within a narrow range to allow body functions to operate).
Dr Brennan is highly trained and experienced in the surgical treatment of conditions of the brain including pituitary tumours.
Conditions:
It is not uncommon for tumours or tumour like processes to develop in the pituitary gland, including pituitary adenoma, Rathke’s cleft cysts, craniopharyngioma, and rarer lesions.
Pituitary adenoma
These tumours are benign, not cancerous, and may cause no symptoms whatsoever if they are incidentally detected on MRI done for some other reason. However, in some cases even though these tumours are benign they can still cause considerable problems in a number of ways.
1. Over production of hormone leading to so-called “endocrinopathies”.
The tumour cells may not be as responsive to the various controls and feedback loops that act on the normal pituitary gland itself. This means that too much of a particular type of hormone may be produced, the exact type depending on which subset of individual cells in the pituitary have turned into the tumour. Although these tumours may become large they are often small, with a lesion less than 1 cm being defined as a microadenoma (and conversely one greater than 1 cm being a macroadenoma). The presence of too much hormone can lead to unusual and widespread effects in the body and both short and long term deleterious effects on health. Examples include Cushing’s disease where there is too much cortisol, gigantism or acromegaly where there is too much growth hormone (in children and adults respectively), and galactorrhea (spontaneous milk production from the breast) with possible infertility if there is too much prolactin hormone. Over and above the discomfort of the initial symptoms some of these conditions, particularly Cushing’s disease and acromegaly, can be fatal if not properly treated.
This is due to the long term downstream effects of the excessive hormone over time leading to morbidities such as diabetes, osteoporosis, hypertension, heart disease, stroke, etc – even though the underlying cause is a benign non-cancerous tumour. As such, so called “secretory” or “functioning” pituitary adenoma almost always needs to be treated.
2. Damage to surrounding structures due to the size of the tumour – so-called “mass effect”.
If the tumour does not produce an active hormone (sometimes called a “non-functioning” adenoma) it may grow to a large size before it declares itself due to compression of adjacent structures.
The pituitary gland itself may become damaged by being crushed by the mass leading to lack of sufficient hormones in the body (a condition called “hypopituitarism”) that may be mistaken for symptoms of ageing including lethargy, listlessness, hair loss, loss of libido, and various other body changes. Further, if the tumour grows upwards and out of the pituitary fossa it may compress the optic nerves leading to various patterns of visual loss, the textbook example being a bitemporal hemianopia due to compression of the optic chiasm.
Again, this may occur gradually and initially be mistaken for the need for glasses although the pattern of visual loss can usually be readily detected by assessment of the visual fields by the doctor or optometrist. Depending on how much damage has already occurred the loss of vision may not recover even after treatment of the tumour, and hypopituitarism is usually permanent (since once the gland fails in rarely recovers again) and may therefore require lifelong hormone replacement.
If sufficient mass effect exists therefore these tumours will also almost always need to be treated.
3. Pituitary Apoplexy.
In most cases damage from mass effect occurs gradually over months to years meaning that symptoms may slowly evolve over time. However, in a small number of cases the tumour may suddenly expand either because it bleeds into itself or out grows its own blood supply and internally dies and hence swells up. The body tissues are generally much less able to cope with a sudden change than a gradual one, and so in severe cases the rapid expansion of the tumour can lead to sudden visual loss, double vision, pituitary failure and collapse. This can be a medical and surgical emergency, but thankfully is not very common.

Treatment options vary considerable depending on the diagnosis and the results of the initial investigations.
Rathke's Cleft Cyst
The normal space between the anterior and posterior lobes of the pituitary is referred to as Rathke’s cleft and is a leftover of the extension from the mouth and nose in the embryo forming the anterior pituitary known as Rathke’s pouch. In some situations the cells which line this space may secrete fluid leading to the formation of a cyst, either in the cleft itself or elsewhere if some of these leftover cells are “trapped” as the gland develops.
Although these cysts may not change at all over time, in other cases the cysts may gradually expand as more and more fluid is secreted by these cells. In this way, although the lesions are not in fact true tumours, the increase in size of the cyst may lead to problems of mass effect as described above for pituitary tumours. In this setting, surgery surgical treatment may be needed to drain the fluid and debride the cyst wall.
Craniopharyngioma
Like Rathke’s cleft cysts, these lesions are not true tumours but may behave as such due to their tendency to gradually get larger and compress and insinuate themselves around the structures in the suprasellar cistern and base of the brain. They are thought to arrive from cells that started as part of Rathke’s pouch but undergo partial changes into a more aggressively growing cyst.
The lesions can occur in many locations in or around the pituitary, as well as higher up towards the brain and even within the fluid compartments of the brain itself. They occur more commonly in children in the first decade of life although a different subtype can occur in adults most commonly in the fifth decade. They often require combinations of treatment such as surgery, medications, and sometimes radiotherapy.
Rarer lesions
A wide variety of less common pathologies can occur in the pituitary region including:
- Other primary tumours such as granular cell tumour and the very rare malignant pituitary carcinoma.
- Meningioma (arising off the lining of the sella)
- Other cysts such as arachnoid cysts and so called “inclusion cysts” such as dermoid and epidermoid cysts
- Metastases (e.g. from breast cancer or lung cancer)
- Germ cell tumours (particularly germinomas in children)
- Infections (pituitary abscess)
- Medical conditions with inflammation (such as lymphocytic hypophysitis, sarcoidosis, etc).
Workup and Investigations
The optimal management of pituitary lesions more often than not requires a team approach between a number of different medical specialists, both before, during, and after treatment.
A careful and thorough assessment is needed to determine what might be going on and help decide on the best treatment options. Most patients can expect to need to have a magnetic resonance imaging (MRI) scan as the key radiological test to sort out the anatomy involved, often supplemented by CT scan particularly if surgery may be needed. Visual function can be assessed by physical examination including the visual fields, visual acuity, and by looking into the back of the eye with an ophthalmoscope. Often, this is supported by review by an ophthalmologist (a doctor specialising in diseases of the eye).
The function of the pituitary gland can be checked with a variety of blood tests most often with the help of an endocrinologist (a doctor specialising in diseases of hormones and metabolism). In more complex cases additional hormone assessment may be needed from urine collections and on some occasions inpatient tests done in hospital to challenge the pituitary and measure its responses (sometimes via a type of angiogram referred to as petrosal venous sinus sampling). Not all of these tests will be required in every case and each patient needs an approach tailored to their on individual issues.



